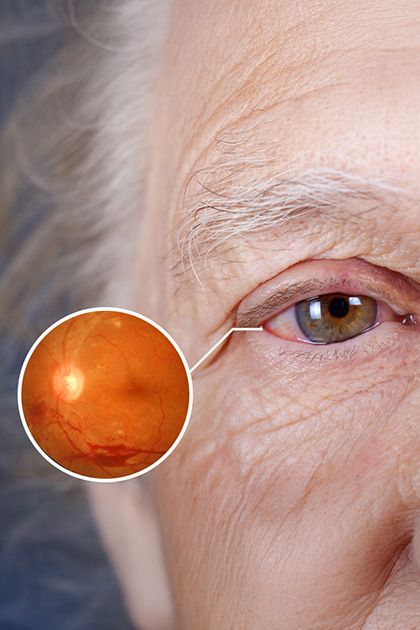

Diabetic Retinopathy is a serious eye condition caused by damage to the blood vessels in the retina — the back layer of the eye — due to long-term diabetes. It may not show symptoms in its early stages but can lead to permanent vision loss as it progresses. With regular eye exams and proper treatment, vision can be preserved.
Occurs in both Type 1 and Type 2 diabetes patients.
The risk increases with the duration of diabetes.
More common in individuals with poorly controlled blood sugar.
Symptoms include blurred vision, decreased night vision, and sudden vision loss.
In early stages, monitoring and blood sugar regulation may be sufficient.
In advanced stages, laser therapy, intravitreal injections, or surgical intervention may be needed.
Early detection is possible through regular retinal exams.
Preventive: Early diagnosis and monitoring help prevent permanent vision loss.
Multifaceted: The treatment plan is customized based on the stage of the disease.
Before procedures such as laser therapy or injections, local anesthesia is applied with eye drops. No pain is felt during the procedure.
The most effective preventive measure is to keep blood sugar levels balanced. Good glycemic control helps slow the progression of the disease.
Leaking weak blood vessels are sealed with a special laser to stop the bleeding and prevent vision loss.
Anti-VEGF medications injected into the eye help reduce vascular leakage and prevent the formation of new, harmful blood vessels.
If there is bleeding in the retina or a retinal detachment, the gel-like substance (vitreous) inside the eye may be surgically removed.
